Corewell Health is the new name for Beaumont.
Corewell Health is the new name for Beaumont.
The learning experience is split over three years. The experience begins with an orientation month with focused lectures, shifts in the emergency department, and a team building retreat. During your training, you will spend most of your time in the emergency department, learning what matters most. Months spent outside of the Emergency Department are heavily focused on critical care. A total of 7 months of exposure to critical care medicine will prepare you to take care of whatever comes through your doors.
Rotation GridLearn more about your comprehensive education in Emergency Medicine that will take place in our large, state-of-the-art Emergency Center which opened in 2019. The center is the statewide leader in Emergency Medicine visits and has over 135 patient beds to accommodate increasingly large volumes of sick patients. The Emergency Center is ACEP geriatric accredited, has a dedicated psychiatric treatment area, as well as a dedicated Pediatric Emergency Center which sees over 23,000 patients in a kid-friendly environment.

You will benefit from working alongside fellowship trained Pediatric Emergency Medicine faculty within our on-site Children's Hospital. Not only will you have several dedicated months of Pediatric EM in your first and second year, along with a PICU experience in your PGY2 year, but you will also have integrated shifts in the Pediatric Emergency Center throughout your training. This will allow you to take advantage of the full depth and breath of pediatric acute care.

The population of older adults is growing rapidly with US adults ≥65 projected to double to 83 million by 2050. The population of the oldest old, aged ≥85, will triple in the same period. At Beaumont Royal Oak, roughly 30% of our
volume is made up of geriatric patients, with 70% of these patients being admitted. Older adults often have multiple medical problems, atypical presentation of diseases, and cognitive impairment. They often require additional resources,
lab testing, and imaging.
At Beaumont, we have made caring for older adult patients a priority and are accredited by the American College of Emergency Physicians as a Level 2 Geriatric Emergency Department. On shift, residents work with our intradisciplinary team to create the best care plans for their patients. Their education is supplemented by a longitudinal lecture series focusing on the different domains of Geriatric Emergency Medicine, innovative simulations, and interaction with the Geriatric Emergency Medicine Fellow, whether on shift or during formal teaching sessions. Additionally, residents have the opportunity to be involved in geriatric research projects, initiatives, and committees both at the hospital and national level. This ensures our residents receive a comprehensive education, allowing them to optimally care for older adults upon graduation.
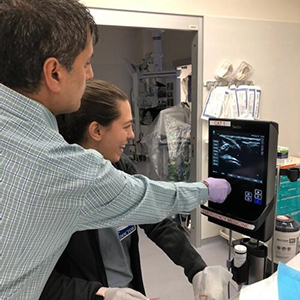
Clinical ultrasound has become an increasingly important tool in the evaluation and Ultrasound treatment of emergency department patients. Our Ultrasound program was developed to train emergency physicians in the utilization of this important diagnostic modality.
Residents are trained in this discipline by expert faculty using fourteen state-of-the-art ultrasound machines. We have two ultrasound fellowship trained faculty on staff along with a robust fellowship program. The majority of our staff are credentialed in a variety of core ultrasound applications and regularly perform studies on clinical shifts.
Residents will have an opportunity to learn this discipline in a variety of ways. The educational curriculum has two blocks of time carved out in the PGY1 and PGY2 year for dedicated ultrasound experiences. The rotations include hands on scanning supervised by expert clinical faculty, image review, journal club, and monthly ultrasound didactic conference. Residents also receive several grand rounds lectures throughout the academic year, participate in procedure labs and attend regional US conferences. This broad exposure translates into seamless use of ultrasound effectively while on clinical shifts. Our residents graduate having completed between 300 and 500 ultrasound studies
Research and scholarly activity are important components of the ultrasound program. Faculty are active at the regional and national level with a number of peer-reviewed publications and grant-funded projects with key areas of interest including: ultrasound-guided vascular access, cardiac ultrasound, and trainee education. Residents have the opportunity to engage in the research process and learn from expert faculty.

As a Level I Trauma Center and a tertiary referral center there is no shortage of critically ill patients. Our residents spend a total of six months on intensive care units acting as junior and senior residents taking care of patients with autonomy. They also get the opportunity to become a critical care specialist within our department during the resuscitation rotation.
The research and resuscitation rotation is built into the PGY-2 curriculum. It is a one month rotation where residents spend time in the high acuity area of the ED assisting with taking care of the sickest patients and performing procedures. The rotation includes weekly meetings to discuss up to date literature and evidence based medicine.

Education in trauma care includes both opportunities within our Emergency Center, the Trauma surgical ICU, and the Trauma Service at Sinai Grace. This well-rounded experience allows ample exposure to critically injured patients along with the added dimension of allowing our residents to experience a different hospital system and patient population.
As the only level 1 trauma center in Oakland County, residents will have ample exposure to Trauma. In addition to resident exposure to critically injured patients during EM months, residents will have a well-rounded experience with a downtown rotation at either Sinai Grace or Detroit Receiving. This allows for an urban trauma experience with the added dimension of experience in a different hospital system and patient population.

How Residents are Evaluated
EM residents at Beaumont are evaluated and provided with feedback in multiple ways. First, residents receive feedback on every EM shift verbally from faculty, and in electronic form using Shift Feedback Cards. Also, a summative evaluation is completed at the end of each rotation in the ED and off-service rotations. Residents also are evaluated once yearly by a nurse and a patient. Finally, residents undergo comprehensive evaluation twice a year by the Clinical Competency Committee, and these findings are discussed with each resident individually at a meeting with the Program Director or Associate Program Director.
How Residents Evaluate the Program
Beaumont EM residents assess and provide feedback to the Beaumont EM Residency on multiple occasions and in multiple formats throughout each year. This includes survey feedback in the form of an ACGME annual survey, and an internal EM Residency survey covering all facets of residency training at Beaumont. Residents also evaluate each faculty member in the residency program to give specific feedback on what they do well and where they can improve as educators. Residents evaluate each rotation at the end of the month as well. Finally, Beaumont EM residents have the opportunity to provide verbal feedback to EM program leadership at monthly Residency Advisory Council meetings, quarterly Program Evaluation Committee meetings, and an annual Program Review meeting.

Residents at the Beaumont Emergency Medicine Residency possess a passion for medical education and our residency affords them a variety of opportunities to pass on medical knowledge and to expand their medical education skills. Medical education at Beaumont begins with working with medical students from the Oakland University-William Beaumont School of Medicine. All students from our medical school will rotate through our ED and residents have the opportunity to teach students, both clinically on shift and through a variety of student didactic sessions.

As a resident in our program, you will be provided with robust educational opportunities to solidify your Emergency Medicine knowledge base. EM core content delivery will be the focus of our weekly EM Grand Rounds, monthly journal clubs, and quarterly simulation and procedural review. Residents will have the opportunity to participate as both learners and educators. We currently utilize a hybrid model for educational content delivery including in-person and virtual meetings. We also emphasize varying models of large versus small group sessions based on topic content and best methods for information delivery. We hope to aid our residents in preparation for their EM written and oral boards while allowing a safe space to discuss various topics that contribute to Emergency Department care.
Foundations is a national curriculum that uses a flipped classroom approach along with case-based learning to learn the fundamentals of emergency medicine. Our residents have 1-3 sessions of Foundations a month during Grand Rounds. Residents are assigned the topic and directed to the appropriate materials to prep for the week's flipped classroom. During Grand Rounds, the residents are broken into small groups based on PGY level and work directly with a faculty member to go through several cases that help reinforce what they prepped for the session. Afterwards, our residents are assigned Rosh Review questions that really cement their knowledge.
We have a variety of EM Resident, Faculty, and guest speakers that contribute to the evolving content of Emergency Medicine practice. We also welcome specialty topics that fit the curiosity of our trainees.

Mentoring is a very important part of our residency. Mentoring helps residents gain practice advice, encouragement and support and helps empower the resident. Our residents choose a faculty member to become their mentors about 6 months into their intern
year. This allows the resident time to develop relationships with our many faculty and find one that most aligns with their goals. The relationship is then cultivated over the next 2.5 years. The mentor and mentee meet several times a year to ensure the
resident is on track to graduate and to help in any way, be it wellness, scholarly activity or networking. The faculty member is also best positioned to help the resident if there are any clinical or knowledge gaps. These relationships are both mutually
beneficial to the resident and faculty member and widely praised throughout the residency.

One of the activities our residents take a part of on a monthly basis is our Emergency Medicine Journal Club. Once a month, usually a Wednesday night, the residents will get together to discuss new high impact journal articles in the field of Emergency Medicine. These journal clubs are graciously hosted by our faculty, usually either at their houses or at an activity of their choosing (e.g. bowling, kickboxing, laser tag, etc.). The goal is to keep up-to-date on the latest and greatest information in the field of Emergency Medicine, while also giving the residents a consistent opportunity to get back together in a fun setting outside of the hospital. Journal clubs are always a fun outlet for our residents, while providing an opportunity to maintain the latest information in the field of Emergency Medicine.

The Wilderness Interest group (WILDS) at Beaumont Royal Oak is dedicated to inspiring residents to engage in the outdoors in an educated and safe manner. The focus is on core topics with training and personal readiness for response to emergencies in the backcountry. Our group promotes and engages in the peripheral disciplines of disaster response, international medicine, sports event medicine. We currently run a longitudinal curriculum of monthly Wilderness topic discussions, culminating in a summer hands-on workshops series. We encourage and work with you to attend national trainings, conferences, and support you in obtaining your Fellowship in the Academy of Wilderness Medicine credentialing.
Each resident in-training at our program will participate in longitudinal learning experiences that fall under the umbrellas of Patient Safety and Quality Improvement, EMS and Flight, and Health Equity. These three curriculums were developed with a unique set of learning objectives and patient care goals in mind. We hope to provide every resident with exposure to various resources that allow advancement of medical care in our patient population and our surrounding community. Whether fostering the development of a niche, or simply gaining understanding of the larger picture of emergency care, these curriculums help to broaden the resident training experience.
Our residency patient safety and quality improvement curriculum offers residents a comprehensive experiential learning experience. Residents will actively engage in Patient Safety and Quality Improvement initiatives through a variety of opportunities, including participating in hospital multi-disciplinary meetings and integrating into our culture of safety meetings. Moreover, residents will have the chance to contribute to peer review committees, gaining valuable exposure to issues surrounding patient safety. The highlight of the program is a mentored Quality Improvement project, where residents will develop essential skills in identifying and executing meaningful changes in healthcare practices. These experiences collectively aim to provide a strong foundation and understanding of patient safety and quality improvement principles, benefitting both residents and the overall healthcare system.
Healthcare disparities, as defined by the Centers for Disease Control and Prevention (CDC), is the “preventable differences in the burden of disease, injury, violence, or opportunities to achieve optimal health that are experienced by socially disadvantaged populations.”
Our curriculum includes lectures and SIM sessions centered around our care for marginalized communities. In recent years, these have included focus on
Racial & ethnic minority groups
LGBTQ population
Limited English Proficiency (LEP) population
Incarcerated population
Homeless population
Residents will take part in community activities through EM's partnership with Oakland Street Medicine.
Ensuring our residents graduate with the leadership skills necessary to excel as an emergency medicine team leader is a critical component of our residency curriculum. Our residents have multiple leadership education opportunities across all three years including simulation experiences, resuscitation management, and committee involvement. We have also developed an innovative, longitudinal leadership curriculum which combines high-yield self-directed learning with interactive case-based discussions. The intent is to help our residents develop the skills, resources, connections, and confidence to successfully lead any medical team in the treatment and care of our patients and community.

Emergency Medical Services (EMS) is a unique discipline in emergency medicine compared to any other specialty. EMS is more than just EMTs, paramedics and ambulances, and is an integrated system of emergency care for patients and communities. EMS transports the majority of critical patients to emergency department. EM providers are looked to by the rest of the health care system to coordinate emergency care for patients with trauma, stroke, STEMI, pediatrics, emergency preparedness and many other specialties. EMS providers are the health care providers that make “house calls” and understand the social determinants of health and the out of hospital circumstances that lead to an individual patients’ emergency visit. They also transport 15-20% of all ED patients to the hospital. For all of those reasons, EM providers must be knowledgeable about EMS, understand how the EMS system works, and how to interact with it in their and other communities.
The residency and its faculty at Beaumont have a long history of EMS engagement at the local, regional, state and national level. Residents become engaged in EMS care, beginning with EMS ride alongs during their first month of their residency. Residents interact with EMS providers on a daily basis when patients are transported to the ED. The educational curriculum provides overview lectures, case review sessions and didactic sessions regarding issues that EMSS plays an important role, such as out of hospital cardiac arrest, and emergency systems of care. EM Residents provide online medical direction beginning in their PGY II year, after completing an online training module regarding medical direction. Residents also have a number of options to provide education to EMS students and practicing providers in the community. They also have the opportunity to participate in other EMS administrative, planning and political activities. For the resident with a particular interest in EMS and wishes a more intensive experience, an EMS elective rotation may be arranged and has been uniformly well received. The department has an active EMS and resuscitation research program in which residents are encouraged to be engaged.

Simulation at Beaumont brings forth a wide range of educational opportunities for our Resident Physicians. The highly integrated format is unique at Beaumont through the existence of one of the most advanced medical simulation facilities in North America, the Marcia & Eugene Applebaum Simulation Learning Institute (SLI). Through the resources at SLI, we have access to highly advanced trainers for the betterment of our Residents’ education. High fidelity simulation scenarios begin from intern year and continue throughout residency training. A connection is formed through individual and group-based learning. One of personal reflection with the goal of gaining familiarity to the real clinical world while a group-based understanding of important team related strategies to parallel a successful outcome in a hectic trauma or medical code. The introduction of the Health Disparity Simulation curriculum has further advanced the Resident education. Through important, but less talked about topics, our Health Disparity Simulation curriculum sheds light on vulnerable patient populations or social considerations or focuses on the Art of Medicine or soft signs of Physician-Patient relationship.
We believe that as physicians our role is not limited to the care we provide in the emergency department. We are community leaders and advocates for our patients inside and outside of the hospital. To provide excellent care for our patients, we need to
develop strong relationships with our community and recognize the needs of our specific patients. Our faculty and residents are actively engaged in several programs to serve our community and patients. On a weekly basis, we provide medical care to
our homeless population outside of the hospital through our Street Medicine Oakland program in collaboration with OUWB. We have the opportunity to recognize their specific barriers to care, and we are able to bring that knowledge back to the care
we are providing in our emergency department. Additionally, we are actively involved in the local schools providing age-based education to both elementary and high school students. Our commitment to service has far-reaching effects both on our community
as well as our own personal wellness.
Learn more about our optional tracks offered for residents interested in creating a niche within our emergency medicine program.
To provide a two-year immersive experience in the field of geriatric emergency medicine; covering in further depth the eight domains of emergency medicine, the identification and management of geriatric syndromes, and development and coordination of intradisciplinary treatment plans for complex older adult patients.
The WHO
The WHY
PGY2 Quarter 1 or before
PGY2 Quarter 2
PGY2 Quarter 3
PGY2 Quarter 4
PGY3 Quarter 1
PGY3 Quarter 2
PGY Quarter 3/Quarter 4
Any questions please contact: Director of Emergency Medicine Research, carol.clark@corewellhealth.org
Other contacts: aveh.bastani@corewellhealth.org, robert.swor@corewellhealth.org
The aim of this track is to provide residents the opportunity to explore academic medicine in the niche of resuscitation and critical care and to develop an enhanced understanding of in-ED clinical resuscitation principles (what to do & what not to do). The residents completing the Resus/CC track will cultivate expertise within multiple realms: cardiac arrest / post-arrest care, pulmonary embolism, cardiac rhythm disturbances, acute MI, sepsis, neurologic emergencies and airway management and hemodynamic stabilization in peri-intubation period.
For those residents who wish the opportunity to have a more focused experience, the residency will now offer a longitudinal track focused on EMS. EMS Medicine has the largest number of ABEM certified subspecialists. For a resident interested in Disaster Medicine, this track will offer a foundational experience on which they resident may build.
The Pediatric Emergency Medicine (PEM) track within the Emergency Medicine residency program is an opportunity for motivated residents to have a longitudinal experience and gain a better understanding of the growing field of pediatric emergency medicine. The curriculum encompasses didactic education, clinical experiences, and hands-on training to prepare residents for the unique challenges of caring for pediatric patients in emergency settings.